In the UK, medical research has helped halve annual deaths from cardiovascular disease since the 1960s – now projects like these are taking heart health into the future
British Heart Foundation (BHF) has been helping to transform the treatment of heart disease since 1961. Relying on public donations, it is the largest non-commercial funder of cardiovascular research in the UK. BHF has invested over £1.5 billion since its inception, which has helped develop medications, surgical techniques and medical devices that have saved countless lives around the world, and it has contributed to a nearly 50 per cent decline in annual cardiovascular disease death rates in the UK since the 1960s.
BHF urgently needs your support to develop this lifesaving work, and by far its biggest source of income comes from legacy giving. BHF collaborates with universities, hospitals and research institutions across the country to support cutting-edge research, and at any one time is funding over 700 potentially transformational projects. Here is just a small sample.
Rewriting history one gene at a time
Professor Hugh Watkins leads the CureHeart project, a £30 million international research programme funded by BHF that aims to change the future for those with inherited heart muscle diseases, or genetic cardiomyopathies, using advanced genetic therapies.
People with cardiomyopathy often live shorter, impaired lives, and many are at high risk of dangerous heart rhythms, stroke and heart failure. And it’s more common than you might think. One in every 250 people is affected – that’s an estimated 260,000 in the UK and 32 million around the world. “Every GP surgery will have several patients with these conditions,” Professor Watkins told The Times in February 2023. Half of all heart transplants are the result of inherited heart muscle diseases.
These diseases come about due to a single “spelling mistake” in a gene, often inherited. None of the current treatments address the root cause. “We know in exquisite detail the exact cause of these conditions, and have created new tools that allow us to correct mistakes in human DNA. We want to use those to fix the fundamental spelling mistake in the gene and restore that back to normal in the heart,” Professor Watkins explains.
His team’s ambition is to develop an injection that either silences the faulty gene or rewrites DNA to correct the genetic spelling mistake. The researchers believe they can cure genetic cardiomyopathies for millions of people, or stop symptoms ever taking hold in the first place.
“The funding from British Heart Foundation is a step change,” Professor Watkins says. “This is what will enable us to hopefully achieve something I never really thought would happen during my career: to come up with cures for these conditions. Then we could see a really transformational impact for these patients and families that we’ve looked after for such a long time.”
Older patients – bigger picture
Following a heart attack, patients often need investigation with an angiogram. Also known as a cardiac catheterisation, this is a heart test that looks at the blood supply of your heart. It helps the doctor spot any narrowings inside the coronary arteries.
But figures from England, Wales and Northern Ireland suggest just 14 per cent of patients over 85 who have a heart attack due to a partially blocked coronary artery have an angiogram, compared with 83 per cent of under-65s. While some older people might be more at risk of complications from treatments, some may be being denied access to these treatments when they could save or improve their lives.
Professor Vijay Kunadian and her team at Newcastle University are trying to address this. “With the outcomes of our findings, we hope to standardise care across the board,” she says.
BHF is funding Professor Kunadian for a clinical trial in which older heart attack patients will either receive medication or medication plus angiogram, and a stent or heart procedure if that’s the best thing to do. It aims to improve guidance for the treatment of older heart attack patients. “Without the funding of BHF, we will not be able to deliver the study,” says Professor Kunadian. “This could impact patients across the UK and the world.”
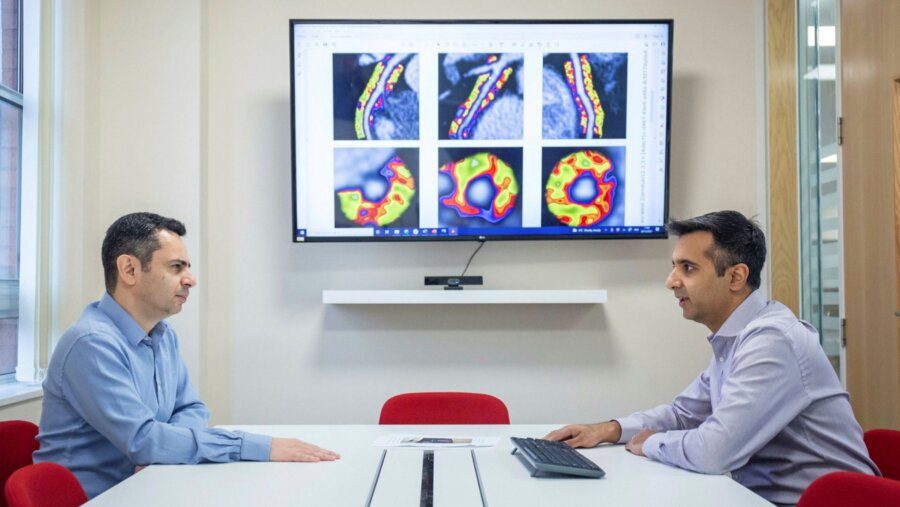
Predicting the risk with the help of AI
Around 350,000 heart CT scans are performed in the UK each year for people experiencing chest pain. Blockages of the heart’s arteries are a major cause, but around 80 per cent of those who undergo a CT scan will show no clear sign of this, suggesting that no further treatment or monitoring is required. Unfortunately, many will, later in life, experience a heart attack (even death) due to small, undetectable narrowings which may end up breaking up when inflamed, causing a blockage in the arteries.
In Oxford, a BHF-funded study is looking to improve the effectiveness of CT scans in assessing the risk of a future heart attack (or cardiac events), ultimately permitting early interventions for many patients. Here, Professor Charalambos Antoniades has developed a new artificial intelligence (AI) tool that can spot early warning signs that are missed by the human eye.
Researchers are validating the AI tool on data from over 80,000 patients. Early research suggested that, for those tested with the tool, heart attacks could be reduced by 20 per cent, and cardiac deaths and strokes by 8 per cent. “We hope this AI tool will be implemented across the NHS, helping prevent thousands of avoidable deaths,” says Professor Antoniades.